Taiwan’s universal health insurance system is known for its high coverage and accessibility, but with the rapid development of medical technology, there has always been a critical “window period” between the speed of launch of innovative drugs (especially specialty drugs) and the review of health insurance benefits. During this period, drugs have been approved for marketing by the competent authorities, but have not yet been included in the health insurance benefits, which poses a heavy economic and psychological burden to patients and their families in urgent need of treatment, and also poses challenges to the market access strategies of pharmaceutical companies.
The Central Health Insurance Administration of the Ministry of Health and Welfare recently announced that it is expected to expand the payment of a number of drugs on June 1, 114 of the Republic of China, including cancer immunotherapy drugs, Olaparib ingredient targeted drugs for the treatment of ovarian cancer, pancreatic cancer, prostate cancer and breast cancer, Bevacizumab ingredient targeted drugs for the treatment of ovarian cancer, and Palivizumab a monobody for the prevention of respiratory fusion virus (RSV) in preterm infants. Most of these drugs are important components of Patientsforce’s current Patient Assistance Program (PAP) to help patients access treatment at their own expense. This move undoubtedly brings hope to patients who have been waiting for a long time, but it also highlights once again that there are still many obstacles between the approval and the widespread adoption of new drugs.
Overview of Taiwan’s specialty drug market and the long wait for health insurance benefits
Taiwan’s pharmaceutical market presents a dual-track nature of health insurance and self-payment. Due to their high unit price and disease-specific characteristics, specialty drugs occupy an important place in the self-pay market. According to Patientsforce’s internal data, nearly 100 patient medication support programs for special drugs in the Taiwan market are in operation, most of which are carried out in the mode of self-paid drug purchase with free drugs or drug fee support, indicating the activity of the self-funded market and the urgent need of patients for innovative treatments.
However, the process of including new drugs in health insurance benefits is often quite lengthy. Pharmaceutical companies can only apply for benefits to the National Health Insurance Administration after obtaining a drug license from the Taiwan Food and Drug Administration (TFDA). The subsequent review process, including the MedicalTech Assessment (HTA), expert meetings, and the PBRS (PBRS) for drug delivery programs, involves multi-party consultation and rigorous evaluation. According to the analysis of data from previous studies, it may take more than 400 days on average for a new drug to be officially covered by health insurance, and the waiting period for cancer drugs may even exceed 700 days. Although the NHSD has made efforts in recent years to speed up the review process, such as promoting parallel reviews for some medicines, with the goal of shortening the timeline to 6 to 10 months, unpredictable delays and case-by-case discrepancies remain. This “window period” can reduce the opportunity for patients to be treated at the most appropriate level, and it also brings uncertainty to the market layout and revenue expectations of pharmaceutical companies.
An accelerator for pharmaceutical companies to enter the market and a guardian network for patients
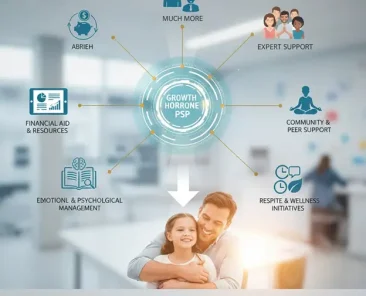
Faced with the window period before the health insurance payment, as well as the possible quota restrictions or special conditions after the health insurance payment, Patientsforce’s PAP program provides a comprehensive solution for pharmaceutical companies and patients.
Value to Pharmaceutical Companies:
- Compliant and fast self-pay market entry: Under the premise of strictly complying with laws and regulations, assist pharmaceutical companies to quickly deploy the self-pay market, reach out to early users, and build brand awareness.
- Flexible support system: We provide a standardized, modular, and parameterized support system. The system can flexibly adapt to the operating procedures of different levels of hospitals, the prescribing habits of physicians, and the individualized medical needs and financial status of patients.
- Improving the accessibility and affordability of medicines: Lowering the threshold for patients to use drugs and expanding the scope of access to drugs through drug cost support and drug gifts.
- Flexible drug cost sharing scheme: For drugs that are partially covered by health insurance or have a maximum payment limit, a model of “early entry and later support” can be designed, such as subsidizing the patient’s out-of-pocket payment difference, or providing support after the annual benefit amount is exhausted.
- Real-world data accumulation: The implementation of the PAP program helps to collect real-world data (RWD) and evidence (RWE) after the patient’s medication, which is highly valuable for subsequent health insurance negotiation, market strategy adjustment, and even academic research.
Value to Patients:
- Reduce financial pressure: Directly lower the financial threshold for self-financed drugs to avoid the “financial toxicity” of poverty due to illness.
- Early access to innovative treatments: No more waiting for health insurance benefits to delay the golden opportunity for treatment.
- Improve treatment adherence: Consistent medication supply and financial support help patients complete their treatment as prescribed, improving treatment outcomes.
Market innovation in pharmaceutical accessibility
In the foreseeable future, with the advent of more high-priced innovative drugs, the limited resources of health insurance and the rigor of review will make the “payment window period” the norm. Against this backdrop, the strategic value of the PAP program is becoming increasingly prominent:
- Key enablers of market access: Patientsforce helps pharmaceutical companies stay ahead of the market in a highly competitive market by shortening the time from time to market to actual sales.
- Maximizing the Lifetime Value of Drugs: From self-funded market education in the early stages of marketing to supplemental support after health insurance benefits, PAP programs can effectively extend the market vitality and revenue contribution of drugs.
- Robust market demand: The continued demand for innovative treatments and financial support provides a stable market foundation for PAP services.
- Enhance corporate social responsibility and brand image: Giving back to the society through the PAP program and helping patients in need is a concrete embodiment of the company’s corporate social responsibility (CSR) practice, which can effectively enhance the company’s public image and brand reputation.
The gap period is a common challenge faced by the medical industry, and through professional, compliant, and innovative patient medication support programs, it can effectively build a bridge between pharmaceutical companies, medical institutions and patients, and shorten the waiting period for patients to receive innovative treatments
Note: The review schedule for the inclusion of new drugs in health insurance benefits varies from case to case, and the number of days cited here is the average or median value mentioned in past academic studies or industry reports, and the actual situation is subject to the official announcement of the Health Insurance Administration. Some of the data is quoted from:
- Lin, Y. J., et al. (2018). New Drug Reimbursement and Pricing Policy in Taiwan. Journal of Forming Medical Association. (Cancer drugs are mentioned on average 742 days)
- Chen, L. F., et al. (2020). Reimbursement Lag of New Drugs Under Taiwan’s National Health Insurance System Compared With United Kingdom, Canada, Australia, Japan, and South Korea. Clinical Therapeutics. (Mention the median of the second generation of health insurance is 458 days)
- Announcement of the Central Health Insurance Administration of the Ministry of Health and Welfare (referring to the target schedule of parallel examination).
- Health insurance new system in June|Expanded benefits for immunotherapy, targeted ovarian cancer and other 4 cancers, Zhixin News 2024/6/1 https://www.knews.com.tw/news/F3C18771F145FB272E60F41847BB33F1