Since its inception in 1995, Taiwan’s National Health Insurance (NHI) system has achieved nearly 100 percent (99.9%) coverage of the insured population with its single-payer model, however, Taiwanese household out-of-pocket expenses (OOPs) account for about 30 %至35% of current health expenditure (CHE), although private insurance coverage is not excluded. However, according to a recent survey by Health Magazine, more than 70% of people have experience with self-financed medicine.
Taiwan’s overall health care expenditure as a percentage of gross domestic product (GDP) has remained around 6.8% for a long time, significantly lower than the average of the Organisation for Economic Co-operation and Development (OECD) countries (about 9.7%)以及鄰近的南韓(約9.3%). )。 However, due to the introduction of new and high-priced medical programs, the complexity of the assessment of benefits included in health insurance and the limitation of total financial resources, the demand for “non-insurance benefits” is increasing, and because Taiwan does not adopt a co-payment system, it is different from the situation in many developed countries where OOP is mainly driven by high partial burden.
The main factors contributing to the increase in out-of-pocket drug bills in Taiwan may include:
- Gap in the payment of new drugs and new technologies: Due to the total annual budget of health insurance, many innovative therapies or drugs that are clinically effective but expensive cannot pass the economic benefit assessment of medical technology, and may be valuable to specific patients, but still cannot prove to have public benefits.
- Difference burden or increase in fully self-pay items: Patients who choose specific medical products with more advanced functions and higher prices are responsible for the difference. If there is no price difference in the new drug section, you must pay for it all out of pocket.
- Limitations or exclusions of health insurance benefits: Health insurance benefits are limited by total or budget considerations, and many restrictions or scopes are given on the condition of payment, so that some patients still have to pay out of pocket.
As Taiwan faces the dual pressures of an aging population and rapid medical technology (high costs), and the overall medical insurance expenditure as a proportion of GDP is low, the pressure on out-of-pocket expenses is bound to intensify. Can international experience provide a solution? The recent ACCESS USA 2025 conference in Philadelphia, USA, brought together global experts in the fields of patient assistance, market access, and special disease care, and discussed topics and trends that are of great value to Taiwan.
ACCESS USA 2025 Global Trends: Implications for Taiwan
ACCESS USA 2025 reveals a rapidly changing area of patient support, driven primarily by policy pressures (such as the U.S. Inflation Reduction Act (IRA), funding challenges, and technological innovation. A few of these core themes may have implications for Taiwan’s situation:
- Matrix Support Program: Beyond Traditional Financial Assistance
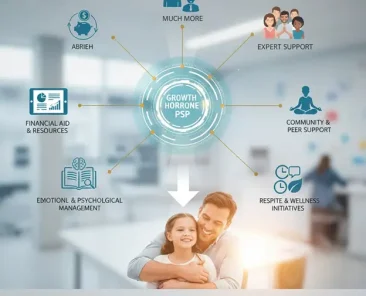
In the face of uncertainty about the future of healthcare and market development, one of the promising developments is the emergence of the “Matrix Support Program” – a comprehensive model that takes into account the multifaceted needs of patients at the same time. Unlike traditional PAPs, which primarily focus on medication shortfall (copay), these comprehensive plans combine:
- Product Acquisition Help (Financial Support)
- Procedural Coverage Support
- Therapeutic Journey Navigator
- Patient treatment effectiveness and adherence plan
For Taiwan, while Medicare provides most of the new drug coverage, there is still a gap in time and space for specific medical care, and the adoption of this matrix support model may significantly improve patient outcomes. By integrating support throughout the treatment journey, these programs can help Taiwanese patients not only overcome the financial aspects of medical care, but also better cope with the complex healthcare system itself.
A matrix approach to Taiwan could include coordinated support from drugmakers, hospital systems, and patient advocacy organizations – creating a safety net that complements the health care structure while addressing its limitations in high-cost therapies.
- Evolution and sustainability of Patient Support Programs (PAPs): Traditionally, PAPs have provided a safety net for the uninsured or under-insured. The meeting highlighted the need for PAPs to evolve to ensure their sustainability and effectiveness. The much-discussed phenomenon of alternative support programs (AFPs) in the United States – the controversy over the program to reduce employer costs by directing insured people to PAPs – operates differently than Taiwan’s, but still has its market innovation value: any aid mechanism, including Taiwan’s growing PAPs/PSPs, requires rigorous design, clear eligibility criteria, and effective oversight to prevent misuse of resources and ensure that aid actually goes to those in need. At the same time, it gives consideration to the incentives of the partner and addresses the patient support interests of specific groups.
- AI & Digital Tools: Empowering Efficiency and Personalization: Artificial intelligence (AI) is seen as a “must-have” technology for patient support by 2025, not a concept of the future. Applications explored include:
- Improve operational efficiency: Automate administrative tasks such as payment verification and pre-event review.
- Personalized interactions: Leverage AI to analyze patient data, predict risks (e.g., medication compliance, financial hardship), and provide tailored communications and interventions. Causal AI was specifically mentioned to understand the “why” behind behavior.
- Proactive support: Predictive analytics and sentiment analysis to identify patients in need of assistance early.
- Patient Journey Tracking: Get a complete picture of your patient’s condition, anticipate needs, and provide guidance.
For Taiwan, the potential of these technologies is huge. AI will not only optimize the operation of PAPs, but may also drive the development of intelligent patient navigation tools. Imagine a system that integrates health insurance regulations, differential burden options, hospital fees, PAPs eligibility, and philanthropic resources to help patients and healthcare professionals identify the most appropriate and cost-effective treatment pathways and address the current information asymmetry.
- Policy Leverage and Market Dynamics: Discussions in the U.S. around the IRA (including a $2,000 OOP cap, drug price negotiations, and installment payments for Medicare Part D drugs) and PBM reform have highlighted the general global challenge of balancing cost control, encouraging innovation, and ensuring accessibility. The experience of the IRA, whether successful or not, provides a valuable reference for Taiwan’s development of HTA policy and the use of MEAs, reminding policymakers to carefully assess the complex trade-offs and potential impacts.
- Optimizing the Patient Journey: The session highlighted that effective support goes beyond financial assistance and must improve the overall patient experience (PX) and compliance. Key strategies include patient-centered design, personalized digital communications, streamlining processes, and importantly, patient education. Studies in the U.S. have shown that patients’ lack of understanding of insurance and assistance programs often leads to delays in treatment. This echoes the confusion of Taiwanese patients when dealing with health insurance, differential burden, out-of-pocket and PAPs. Therefore, the government should be more open to the market mechanism in the pharmaceutical policy, and the support system must include clear information, convenient navigation and personalized care.
Translating global insights into momentum for Taiwan
The innovative thinking of ACCESS USA 2025 provides concrete directions for Taiwan to address the challenges:
- Strengthening Taiwan’s PAP ecosystem: Taiwan’s existing PAPs/PSPs can be referenced from international practices to improve transparency and ensure compliance (especially personal data protection). The key is to strengthen the integration of PAPs, hospital systems and health insurance systems, so that physicians can more easily initiate assistance applications for patients at the point-of-care endpoint, and establish an integrated model of “hub services”.
- Driving the Digital Transformation of the Health Care System: The potential of AI goes far beyond PAPs. The health insurance system can explore the application of AI to:
- Assists in HTA decision-making (analysis of real-world data).
- Predict high-risk populations to optimize resource allocation.
- Improve administrative efficiency (e.g., automated reviews).
- Develop intelligent patient navigation tools. However, this requires a robust data infrastructure and governance framework to address privacy and ethical challenges.
- Improving policy paths: Drawing on international experience, Taiwan can consider:
- Targeted financial protections: Refer to the spirit of the IRA’s OOP cap and establish stronger protections for specific high-priced out-of-pocket projects or vulnerable groups.
- Optimized Value Assessment: Continuous refinement of the HTA/MEA process with wider use of RWE and results-based payment protocols.
- Dealing with low-value care: Establish mechanisms to review and potentially eliminate low-efficiency health insurance benefits and redirect resources to high-value innovations.
- Improve the supervision of the self-pay market: Strengthen the transparency and regulation of information on the difference burden and the full self-pay project to protect the rights and interests of patients.
- Promote multi-party collaboration: Build a platform to promote dialogue and cooperation among the government, the medical sector, industry, the technology industry and patient groups to find diversified solutions.
From the evolution of PAPs, the application of AI and digital technologies, to the lessons learned from policy change, and the emphasis on the patient experience, these global insights are invaluable. The key is to translate these visions and thinking into localized solutions that are suitable for Taiwan’s unique medical environment.
This includes improving the effectiveness of existing patient support programmes, leveraging technology to empower health care systems and service processes, and carefully balancing multiple objectives at the policy level. The adoption of AI technology has great potential, but it must be accompanied by an equal emphasis on data governance, privacy, and ethics.
Addressing the growing out-of-pocket costs requires the concerted efforts of all stakeholders, including the government, the medical sector, industry, technology partners and patient groups. Through open dialogue, pragmatic planning and innovative practices, and drawing on global wisdom to address local challenges, Taiwan will have the opportunity to further improve its healthcare system, reduce the burden on the public, improve the accessibility and quality of medical care, and ultimately move towards a more sustainable, fairer and more responsive future that better meets the health needs of the whole population.