High-cost drugs for home care and chronic diseases support the demand
In recent years, as medical demand and supply change, the healthcare system is being pushed towards decentralization. In the United States, more and more insurance companies and PBMs (Pharmacy Benefit Managers) are using payment tools such as alternative funding programs (AFPs), copay accumulators and copay maximizers, mainly for the benefit of high-priced emerging drugs to strictly control and pass on financial pressure to pharmaceutical companies, which leads to more obstacles for patients to access treatment.
For example, in the AFPs model, insurance companies may exclude certain high-priced drugs from reimbursement, making it appear as if the patient is uninsured, and then refer them to a patient assistance plan (PAP) to cover the cost of the drug. This has directly led to a surge in PSP’s PAP services, forcing the pharmaceutical industry to respond in a more flexible and scalable way.
Under this financial pressure, the pharmaceutical industry must rethink its PSP model. Traditional fully outsourcing models may not be able to respond to these complex and evolving payment strategies in real-time. Therefore, adopt a hybrid decision-making model and integrate it into internal information systems to better control the patient and HCP experience and gain more comprehensive data insights. This shift in model is in response to the needs derived from the decentralization of hospitals, where the interaction scenarios between patients and HCPs have extended from inside the hospital to outside the hospital.
The Complexity of Home Care: Challenges Beyond Logistics
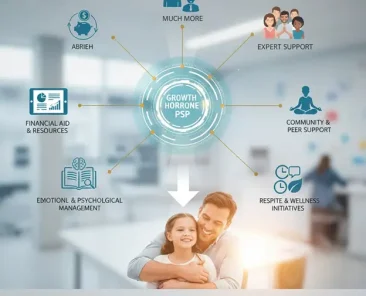
As treatment shifts from the hospital to the home, the patient’s role shifts from passive recipient to active manager, and the challenges faced by PSP escalate. The complexity of home care extends beyond drug logistics and distribution, encompassing multiple aspects such as patient education, medication adherence monitoring, side effect management, and emotional support.
For patients who need to self-inject or infuse at home, PSPs must provide comprehensive instruction and guidance to ensure that patients can administer medication correctly and safely. In the past, most of this education was done by in-hospital nurses or professionals. However, in the home care model, PSPs must fill this service gap through telemedicine, professional nurse home services, or digital tools. The high level of patient satisfaction assisted by nurses in telemedicine is a testament to the indispensability of professionals in home care.
In addition, medication adherence is a core challenge in home care. Without medical supervision, patients can easily forget to take their medication or stop it on their own due to side effects. In the future, PSP integrates artificial intelligence (AI) and data analysis technologies to accurately predict patients who may fall out, and provide timely intervention and support through personalized and multi-channel communication methods to ensure that patients can adhere to a complete treatment course.
Technology empowers to build a new blueprint for PSP for home care
Technology-first: From passive support to active empowerment
Traditional PSPs mostly rely on manpower-intensive services, but this model is difficult to scale in the face of the huge demand for home care. The demand for PSPs that emphasize “technology first” in the report is on the rise. These vendors see technology at the core, not just as an aid.
The concept of a digital hub is one example. Tasks such as e-BV and e-PA can be automated through interoperable technology, reserving human intervention for the most complex and most interactive-seeking cases. At the same time, reducing treatment initiation time allows PSP staff to focus on providing more valuable patient services.
AI and Big Data: The Key to Personalization and Precision
In home care, every patient’s journey is unique. PSPs must be able to provide customized services based on individual needs. AI and big data are the key to achieving this goal.
In the current development of AI in PSP, there are various application scenarios, including operational efficiency improvement, patient coverage determination, personalized patient interaction, and conversational intelligence analysis. For example, AI can accurately predict possible breakpoints based on patient data and deliver the right information at the right time and through the right channel through personalized communication. This not only improves medication adherence but also makes patients feel valued and cared for.
But AI is not everything. In certain scenarios, such as patient coverage determination, AI relies on vast historical data for predictions, potentially risking inaccuracies. Therefore, the combination of directly linked benefit insurance and PSP information can ensure the real-time and accurate data exchange, and the need for information exchange always exists.
Repositioning and new roles of professionals
Talent shortage and digital transformation in medical benefits
While technology plays an increasingly important role in PSPs, the value of professionals has not been replaced. On the contrary, as the complexity of home care increases, so does the demand for PSP talent. Professional PSP personnel not only need to have professional knowledge of diseases, drug delivery methods, insurance design, etc., but also need empathy to address the challenges faced by patients and HCPs in the complex healthcare system.
The talent shortage and work model changes in the post-epidemic era have also brought new challenges to PSPs. Traditional remote work models can lead to uneven service quality. Therefore, PSP providers must provide clear recruitment, training, and performance management processes, and ensure that their workforce can continue to evolve to meet changing market demands.
The new role of professionals: value creators under human-machine collaboration
In the new PSP model of “technology first”, the role of PSP professionals is being redefined. They are no longer mere administrative task performers, but value creators under human-machine collaboration.
With automated Advanced eServices, PSPs can free themselves from tedious paperwork and spend more time having meaningful conversations with patients and HCPs. The implementation of a patient journey management system provides real-time information such as the content of the patient’s medication support plan, prior authorization requirements, deductibles, or PAP eligibility. This allows PSP personnel to quickly grasp the situation as soon as possible and provide warm professional advice.
This model not only improves work efficiency but also allows PSP personnel to focus more on providing empathy and emotional support, a core value that no technology can replace in home care.
For pharmaceutical companies, partnering with professional PSP service providers like PatientsForce not only addresses payer strategy and regulatory challenges, but also establishes a differentiated patient experience and strengthens tripartite collaboration between medicine and disease.
For investors, PSP’s value has transcended the “cost center” and has become a strategic asset driving drug accessibility, patient adherence, and the sustainable growth of pharmaceutical brands. Grasping the development context of PSP after “decentralization” will be the key for every medical professional and investor to stay ahead in the next medical competition cycle.